Iliac-hepatic arterial bypass for
compromised collateral flow during
modified Appleby operation for
advanced pancreatic cancer
Machado MA, Surjan RC, Nishinari K, Makdissi FF, Machado MC.
Eur J Surg Oncol. 2009 Oct;35(10):1124-7.

Machado MA, Surjan RC, Nishinari K, Makdissi FF, Machado MC.
Eur J Surg Oncol. 2009 Oct;35(10):1124-7.
Iliac-hepatic arterial bypass for compromised collateral flow during modified Appleby operation for advanced pancreatic cancer
M.A. Machado‡, R.C. Surjan‡, K. Nishinari*; F.F. Makdissi‡ and M.C. Machado‡
Introduction
Despite advances in chemotherapy and trend towards more aggressive surgical resection, long-term prognosis of pancreatic adenocarcinoma remains poor.1 Involvement of the celiac trunk and common hepatic artery are two of the most common forms of vascular invasion by tumours of the distal pancreas, and until recently this finding was considered a contra-indication to resection. In 1953, Appleby proposed en bloc resection of the celiac trunk with distal pancreatectomy and total gastrectomy for the treatment of locally advanced gastric cancer.2 This operation was first adapted to the resection of tumours of the body and tail of the pancreas in 1976, by Nimura.3 In 1991, Hishinuma performed two distal pancreatectomies with resection of the celiac axis with gastric preservation, named the modified Appleby procedure.1,4
We described a case of a modified Appleby operation for locally advanced distal pancreatic cancer with compromised hepatic collateral flow that needed hepatic arterial revascularization, successfully accomplished by left external iliac-hepatic arterial bypass with Dacron prosthesis. To our knowledge this type of arterial bypass has never been described so far in the English literature and its description may be important for surgeons dealing with advanced pancreatic cancer.
Methods
Preoperative evaluation
A 71-year-old man with pancreatic body cancer after neoadjuvant gemcitabine-based chemotherapy was referred for surgical treatment. Abdominal CT scan was performed and showed a locally advanced tumour (Fig. 1). Complete tumour screening including chest CT and positron emission tomography (PET-CT) was performed and discarded extrapancreatic disease. Laboratory tests were all within normal range, except for increased CA 19-9 level.
Detailed analysis of a sequence of abdominal CT scans performed before the surgical procedure revealed a marked decrease in tumour size after chemotherapy, but the celiac axis remained involved (Fig. 1).
Operative assessment
During surgical exploration, the tumour was confined to the pancreas and nearby structures, and there were no signs of liver metastasis or peritoneal dissemination. Intraoperative palpation of Aorta confirmed the presence of diffuse calcification but left external iliac artery was not compromised (Fig. 1d)
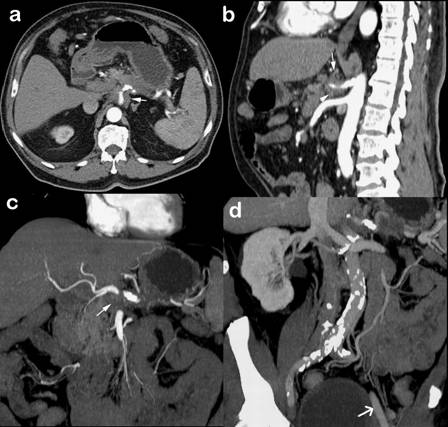
FIGURE 1. Preoperative CT scan.
a. Axial view shows a large tumour in the body of the pancreas involving celiac axis (arrow).
b. Sagittal view shows involvement of celiac trunk (arrows). Mesenteric trunk is free.
c. Coronal view shows tumour in the body of the pancreas with invasion of celiac axis (arrow).
d. 3D reconstruction shows Aorta diffusely calcified. Left external iliac artery (arrow) is spared.
Operative technique
The first step was to dissect the common hepatic artery from the gastroduodenal artery until the macroscopic limit of the tumour. As described by previous reports, since the initial approach to the celiac trunk, proper hepatic artery pulsation was tested several times with the intent to confirm adequate collateral flow by mesenteric arterial branches.5-8 However, when the common hepatic artery was temporally clamped, the pulse of the proper hepatic artery became remarkably weak, indicating that the collateral flow by pancreaticoduodenal branches was insufficient to guarantee adequate hepatic arterial flow and the need for arterial revascularization. Portal vein tunnel was performed and confirmed no tumoural involvement of the vein.
The next step was to perform an en bloc mobilization of distal pancreas and spleen, allowing complete access to celiac axis and superior mesentery artery roots, which were encircled with surgical vessel loop. After complete control of vascular beds, the pancreas was divided along the right side of the portal vein. Splenic vein and left gastric artery were divided. Surgical specimen remained attached to celiac axis and common hepatic artery, so their division would free surgical specimen. Therefore, hepatic arterial flow was maintained as long as possible.
Arterial revascularization
Left external iliac artery was chosen to perform the proximal arterial anastomosis. After administration of intravenous heparin, left iliac artery was clamped and a longitudinal arteriotomy was performed. End-to-side anastomosis between 8 mm Dacron graft and external left iliac artery was then performed. The prosthesis was then passed through the retroperitoneum to reach the superior abdomen near the hepatic hilum. At this moment, the common hepatic artery was divided, and a continuous end-to-end anastomosis was performed between the hepatic artery and the Dacron prosthesis (Fig. 2). Vascular clamps were then released and hepatic arterial flow was re-established. Total arterial hepatic ischemic time was 6 minutes.
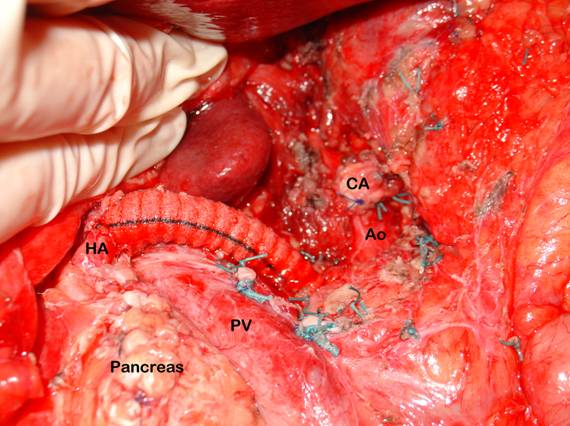
FIGURE 2. Final aspect. Intraoperative photograph shows pancreatic remnant after spleno-pancreatectomy with en bloc resection of celiac axis (CA). Aorta (Ao), portal vein (PV) and hepatic artery (HA) are identified.
Specimen extraction
Celiac trunk was divided and en bloc resection of the tumour, pancreas, spleen and celiac axis was completed. Surgical specimen was then removed. One round 19F Blake abdominal drain (Ethicon, Inc, Cincinatti, Ohio) was left in place.
Results
Outcome
Patient did not receive transfusion and recovery was uneventful. Patient was discharged on the 10th postoperative day. Abdominal drain was removed on the 12th postoperative. Postoperative angio-CT disclosed a patent arterial bypass (Fig. 3). Patient is well and asymptomatic 13 months after operation. At the time of this writing, postoperative CT scan showed no evidence of disease and CA 19-9 level is normal.
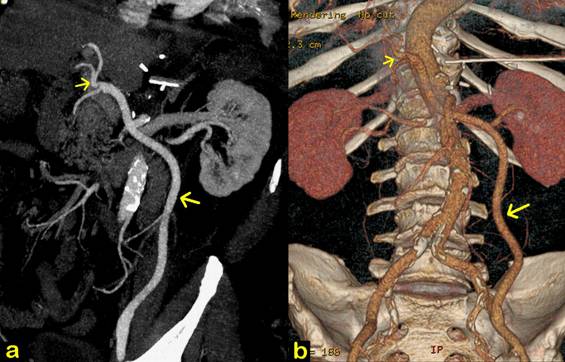
FIGURE 3. Postoperative angio-CT scan.
a. Coronal view shows a patent Dacron vascular graft (large arrow). Hepatic artery is identified (small arrow).
b. Colour 3D reconstruction shows a patent left external iliac-hepatic arterial bypass (large arrow). Hepatic artery is identified (small arrow). Note diffuse calcification of abdominal Aorta and absence of celiac trunk. Abdominal drain can be seen.
Discussion
Background
Modified Appleby procedure has been successfully performed for locally advanced distal pancreatic cancer with involvement of the celiac axis and some long term survivals have been reported.9-11 This technique is also efficient to control abdominal and back pain resulted from involvement of the celiac ganglia by pancreatic tumours.6 Furthermore, several studies have suggested that R0 resections are associated with significant improvement in survival when compared to palliative therapy and that patients submitted to expanded vascular resections nearly equals the survival of standard pancreatectomy patients.9,12
Anatomical considerations
Anatomic basis for this approach is the presence of collateral circulation between the superior mesenteric artery and the hepatobiliary system by an intact pancreaticoduodenal arcade. Since its original report by Appleby, a major concern was to preserve the hepatic arterial flow. Although some authors state that the proper hepatic artery flow is not essential to liver functioning and that it can be transected unpunished in cases that portal vein is not affected by tumour, hepatic arterial flow must be considered as important oxygen source for hepatic metabolism.9
Technical considerations
In this particular case, collateral flow by pancreaticoduodenal branches did not guarantee adequate arterial blood supply to the liver. Moreover, due to extensive calcification, distal aorta, common iliac and right external iliac arteries were not suitable for anastomosis (Fig. 1d). Therefore, we elected the left external iliac artery for proximal vascular anastomosis. Regarding the vascular substitute, safena magna could be an option but it would be prone to excessive kinking or compression on its long retroperitoneal course. A Dacron vascular prosthesis was used instead, and postoperative angio-CT scan shows adequate graft patency (Fig. 3).
Conclusion
There is a well established rationale to perform extended resection of pancreatic carcinomas that compromise vascular structures. Modified Appleby procedure can safely be performed, has oncological advantages to palliative procedures and provides relief of pain but is reserved for selected patients. Preservation of hepatic arterial flow has utmost importance to avoid hepato-biliary complications as liver necrosis, liver abscess, gallbladder necrosis or cholecystitis.3,13 In this case, hepatic revascularization was particularly challenging, but was successfully accomplished by left external iliac-hepatic arterial bypass.
REFERENCES